Determining safe entry sites for filler injections on the lateral canthal vertical line: Anatomical study of the midface arterial perforators in soft embalmed cadavers (2016)
Title : Determining safe entry sites for filler injections on the lateral canthal vertical line: Anatomical study of the midface arterial perforators in soft embalmed cadavers
Researcher : Rungsawang, C., Tansatit, T., Phumyoo, T., Jitaree, B., Uruwan, S.
Abstract : Background: Filler injections are frequently associated with vascular complications.Objectives: To investigate the course and location of the middle-midface perforators to establish safe cannulaentry sites for filler injections.Methods: The middle-midface was studied using 28 hemiface specimens from soft embalmed Thai cadavers atthe Faculty of Medicine, Chulalongkorn University. Investigations were performed following injection of red latex.Results: Middle-midface perforators were classified into 3 groups according to their origin. These perforatorsoriginated from the buccal branch of the facial artery (57%); the parotid artery (25%); or directly from the facialartery (18%). The distance between the buccal artery perforator (level with the upper alar crease) and the lateralcanthal (Y axis) line was 2.6 (SD 6.0) mm and Frankfort’s horizontal (X axis) lines was −16.4 (5.4) mm. The distancebetween the parotid artery perforator and the lateral canthal vertical line was 4.2 (10.8) mm and Frankfort’shorizontal line was −13.9 (3.4) mm. The distance between the facial artery perforator and the lateral canthal verticalline was 11.2 (10.8) and Frankfort’s horizontal line was –16.0 (5.3) mm.Conclusions: A single long perforator was identified along the lateral canthal vertical line. This most commonlyoriginated from the buccal branch emerging from the facial artery. Therefore, we recommend a cannula be insertedat the Beut site 2 cm inferolateral to the lateral canthus. This injection site is recommended as a safe to avoidinjury to the middle-midface perforato
Keywords: Facial artery perforator, filler injection technique, injectable filler complications, midface volumizati
Link to Academic article: https://sciendo.com/article/10.5372/1905-7415.1006.532
Journal : Asian Biomedicine, 2016, 10(6),
Bibliography : Rungsawang, C., Tansatit, T., Phumyoo, T., Jitaree, B., & Uruwan, S. (2016). Determining safe entry sites for filler injections on the lateral canthal vertical line: Anatomical study of the midface arterial perforators in soft embalmed cadavers. Asian Biomedicine, 10(6), 619–625.
Effect of needle sizes 30 G and 32 G on skin penetration force in cadavers: Implications for pain perception and needle change during botulinum toxin injections (2021)
Title : Effect of needle sizes 30 G and 32 G on skin penetration force in cadavers: Implications for pain perception and needle change during botulinum toxin injections
Researcher : Tansatit, T., Uruwan, S., Wilkes, M., Rungsawang, C.
Abstract : Cosmetic botulinum toxin injections usually cause discomfort to the patient. Using a small needle causes less pain compared to using a large needle,1 but a drawback is the price. A 30-G needle costs 2 THB while a 32-G needle costs 15 THB. The physician must decide when a needle is to be discarded. In one study, a 30-G needle was changed after approximately four to six punctures because of increased skin resistance.2 A 32-G needle is less painful than a 30-G needle because of the 25 percent smaller diameter of the 32-G needle.3 Instead of relying on individual tactile sense, we compared the penetration forces of two needle sizes to decide when to change the needle during botulinum toxin treatment.
Link to Academic article: DOI: 10.1097/PRS.0000000000008558
Journal : Plastic and Reconstructive Surgery, 2021, 148(6), pp. 1071E–1073E
Bibliography : Tansatit, T., Uruwan, S., Wilkes, M., & Rungsawang, C. (2021). Effect of needle sizes 30 G and 32 G on skin penetration force in cadavers: Implications for pain perception and needle change during botulinum toxin injections. Plastic and Reconstructive Surgery, 148(6), 1071E–1073E. DOI: 10.1097/PRS.0000000000008558
Localization and topography of the arteries on the middle forehead region for eluding complications following forehead augmentation: Conventional cadaveric dissection and ultrasonography investigation (2020)
Title : Localization and topography of the arteries on the middle forehead region for eluding complications following forehead augmentation: Conventional cadaveric dissection and ultrasonography investigation
Researcher : Phumyoo, T., Jiirasutat, N., Jitaree, B., Rungsawang, C., Pratoomthai, B., Tansatit, T.
Abstract :Forehead augmentation with filler injection is one of the most dangerous procedures associated with iatrogenic intravascular injection resulting in the severe complications. Nonetheless, few studies have determined the explicit arterial localization and topography related to the facial soft tissues and landmarks. Therefore, this study aimed to determine an arterial distribution and topography on the middle forehead region correlated with facial landmarks to grant an appropriate guideline for enhancing the safety of injection. Nineteen Thai embalmed cadavers were discovered with conventional dissection and 14 Thai healthy volunteers were investigated with ultrasonographic examination on the middle forehead. This study found that at the level of mid-frontal depression point, the transverse distance from the medial canthal vertical line to the superficial and deep branches of supraorbital artery were 9.1 mm and 15.1 mm, respectively. Whereas the depths from the skin of these arteries were 4.1 mm and 4.3 mm, respectively. Furthermore, the frontal branch of superficial temporal artery was detectable in 42.1% as an artery entering the forehead area. At the level of lateral canthal vertical line, the vertical distance of frontal branch was 31.6 mm, and the depth from skin of the artery was 2.7 mm. In conclusion, a proper injection technique could be performed based on an intensive arterial distribution and topography, and ultrasonographic examination before the injection is also suggested in order to restrict the opportunity of severe complications.
Keywords: Complication of filler injection , forehead augmentation , frontal branch of superficial temporal artery , superficial and deep branches of supraorbital artery , ultrasonographic investigation
Link to Academic article: https://journals.lww.com/jcraniofacialsurgery/Abstract/2020/10000/Localization_and_Topography_of_the_Arteries_on_the.43.aspx
Journal : Journal of Craniofacial Surgery, 2020, 31(7).
Bibliography : Phumyoo, T., Jiirasutat, N., Jitaree, B., Rungsawang, C., Pratoomthai, B., & Tansatit, T. (2020). Localization and topography of the arteries on the middle forehead region for eluding complications following forehead augmentation: Conventional cadaveric dissection and ultrasonography investigation. Journal of Craniofacial Surgery, 31(7), 2029–2035.
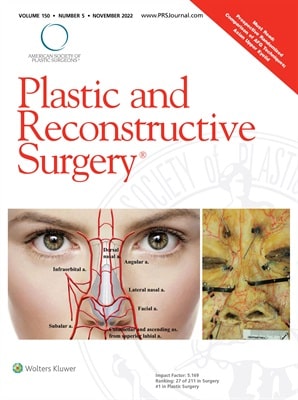
Lower Nose Arterial Plexus and Implications for Safe Filler Injections (2022)
Title : Lower Nose Arterial Plexus and Implications for Safe Filler Injections
Researcher : Tansatit, T., Jitaree, B., Uruwan, S., Rungsawang, C.
Abstract : Background: The lower nose has abundant blood supply; however, nasal tip necrosis still occurs following filler injections. This study revealed the complicated pattern of the arterial supply of the lower nose.
Methods: The arterial pattern of the lower nose was studied in 40 cadavers using conventional dissections and translucent modified Sihler staining.
Results: Two arterial rings were connected in a figure of eight. The upper ring (nasal arterial circle) consisted of the lateral nasal and the subalar arteries encircling the nasal tip and alae. The lower ring (arterial plexus of the upper lip) was more important because of the contribution of the facial and superior labial arteries. This specific feature had not been mentioned elsewhere.
Conclusion: Understanding this specific feature of the blood supply of the lower nose is essential for aesthetic physicians to perform the appropriate techniques during filler injection procedures in the nasal and perioral regions.
Link to Academic article: DOI: 10.1097/PRS.0000000000009649
Journal : Plastic and Reconstructive Surgery, 2022, 150(5),
Bibliography : Tansatit, T., Jitaree, B., Uruwan, S., & Rungsawang, C. (2022). Lower Nose Arterial Plexus and Implications for Safe Filler Injections. Plastic and Reconstructive Surgery,150(5), 987E–992E. DOI: 10.1097/PRS.0000000000009649

The analgesic efficacy of anterior femoral cutaneous nerve block in combination with femoral triangle block in total knee arthroplasty: a randomized controlled trial(2021)
Title : The analgesic efficacy of anterior femoral cutaneous nerve block in combination with femoral triangle block in total knee arthroplasty: a randomized controlled trial
Researcher : Kampitak, W., Tanavalee, A., Tansatit, T., …Songborassamee, N., Vichainarong, C.
Abstract : Background: Ultrasound-guided femoral triangle block (FTB) can provide motor-sparing anterior knee analgesia. However, it may not completely anesthetize the anterior femoral cutaneous nerve (AFCN). We hypothesized that an AFCN block (AFCNB) in combination with an FTB would decrease pain during movement in the immediate 12 h postoperative period compared with an FTB alone.
Methods: Eighty patients scheduled to undergo total knee arthroplasty were randomized to receive either FTB alone (FTB group) or AFCNB with FTB (AFCNB + FTB group) as part of the multimodal analgesic regimen. The primary outcome was pain during movement at 12 h postoperatively. Secondary outcomes included numeric rating scale (NRS) pain scores, incidence of surgical incision site pain, intravenous morphine consumption, immediate functional performance, patient satisfaction, and length of hospital stay.
Results: The NRS pain scores on movement 12 h postoperatively were significantly lower in the AFCNB + FTB group than in the FTB group (mean difference: –2.02, 95% CI: –3.14, –0.89, P < 0.001). The incidence of pain at the surgical incision site at 24 h postoperatively and morphine consumption within 48 h postoperatively were significantly lower (P < 0.001), and quadriceps muscle strength at 0° immediately after surgery was significantly greater in the AFCNB + FTB group (P = 0.04).
Conclusions: The addition of ultrasound-guided AFCNB to FTB provided more effective analgesia and decreased opioid requirement compared to FTB alone after total knee arthroplasty and may enhance immediate functional performance on the day of surgery.
Keywords: Arthroplasty; Knee; Nerve block; Peripheral nerves; Postoperative pain; Ultrasonography.
Link to Academic article: DOI: https://doi.org/10.4097/kja.21120
Journal : Korean Journal of Anesthesiology, 2021, 74(6).
Bibliography : Kampitak, W., Tanavalee, A., Tansatit, T., Ngarmukos, S., Songborassamee, N., & Vichainarong, C. (2021). The analgesic efficacy of anterior femoral cutaneous nerve block in combination with femoral triangle block in total knee arthroplasty: a randomized controlled trial. Korean Journal of Anesthesiology, 74(6), 496–505. DOI: https://doi.org/10.4097/kja.21120

The crest injection technique for glabellar line correction and the paracentral artery (2021)
Title : The crest injection technique for glabellar line correction and the paracentral artery
Researcher : Tansatit, T., Uruwan, S., Rungsawang, C.
Abstract : The glabella is a zone that carries a high risk of blindness after performing filler injections. The arteries beneath the glabellar lines were investigated by meticulous dissections in 30 geriatric embalmed cadavers with latex injections into the arterial system. The results showed that the supratrochlear artery, a direct branch of the ophthalmic artery, ascended from the muscular layer of the medial eyebrow along the medial canthal vertical line of the intercanthal vertical zone (53 in 60 hemifaces, or 88%). The dominant single paracentral artery from the radix artery was found within the radix vertical zone (eight out of 30 glabellae, or 27%). Among these, the dominant paracentral artery was near the midline in two cadavers and arose along the radix vertical line in six cadavers. The dominant paracentral artery may be the cause of ocular complications during injections of glabellar lines between the medial eyebrows, especially at the radix vertical lines. The supratrochlear artery might cause ocular complications when an injection is performed close to the medial eyebrows. Pinching to create a skin crest and evert glabellar line for a precise injection is recommended to temporarily occlude the paracentral artery.
Link to Academic article: DOI: 10.1097/GOX.0000000000003982
Journal : Plastic and Reconstructive Surgery – Global Open, 2021, 9(12).
Bibliography : Tansatit, T., Uruwan, S. & Rungsawang, C.,(2021). The crest injection technique for glabellar line correction and the paracentral artery. Plastic and Reconstructive Surgery – Global Open, 9(12), e3982. DOI: 10.1097/GOX.0000000000003982

The feasibility determination of risky severe complications of arterial vasculature regarding the filler injection sites at the tear trough (2018)
Title : The feasibility determination of risky severe complications of arterial vasculature regarding the filler injection sites at the tear trough
Researcher : Jitaree, B., Phumyoo, T., Uruwan, S., …McCormick, L., Tansatit, T.
Abstract : Background: The tear trough is a significant sign of periorbital aging and has usually been corrected with filler injection. However, the arterial supply surrounding the tear trough could be inadvertently injured during injection; therefore, this study aimed to evaluate the nearest arterial locations related to the tear trough and investigate the possibility of severe complications following filler injection.
Methods: Thirty hemifaces of 15 Thai embalmed cadavers were used in this study.
Results: The artery located closest to both the inferior margin (TT1) and mid-pupil level (TT2) of the tear trough was found to be the palpebral branch of the infraorbital artery. Furthermore, at 0.5 mm along the tear trough from the medial canthus (TT3), the angular artery was identified, which was found to be a branch of the ophthalmic artery. The artery at TT1 and TT2 was located beneath both the zygomaticus major and the orbicularis oculi muscles. The distances from TT1 to the artery were measured as follows: laterally, 2.79 ± 1.08 mm along the x axis; and inferiorly, 2.88 ± 1.57 mm along the y axis. For the TT2, the artery was located inferomedially from the landmark of 4.65 ± 1.83 mm along the x axis and 7.13 ± 3.99 mm along the y axis. However, the distance along the x axis at TT3 was located medially as 4.00 ± 2.37 mm.
Link to Academic article: DOI: 10.1097/PRS.0000000000004893
Journal : Plastic and Reconstructive Surgery, 2018, 142(5).
Bibliography : Jitaree, B., Phumyoo, T., Uruwan, S., Sawatwong, W., McCormick, L., & Tansatit, T. (2018). The feasibility determination of risky severe complications of arterial vasculature regarding the filler injection sites at the tear trough. Plastic and Reconstructive Surgery, 142(5), 1153–1163. DOI: 10.1097/PRS.0000000000004893

Three-dimensional evaluation of the depressor anguli oris and depressor labii inferioris for botulinum toxin injections (2021)
Title : Three-dimensional evaluation of the depressor anguli oris and depressor labii inferioris for botulinum toxin injections
Researcher : Choi, Y.-J., We, Y.-J., Lee, H.-J., …Tansatit, T., Kim, H.-J.
Abstract : Background: Botulinum toxin type A (BoNT-A) injection administered at an inappropriate site or depth can produce an unwanted change in facial animation because the depressor anguli oris (DAO) and depressor labii inferioris (DLI) muscles are partially overlapped. Therefore, simple BoNT-A injection guidelines, based on 3-dimensional (3D) facial anatomic references and landmarks, would be very useful.
Link to Academic article: https://doi.org/10.1093/asj/sjaa083
Journal : Aesthetic Surgery Journal, 2021, 41(6).
Bibliography : Choi, Y. J., We, Y. J., Lee, H. J., Lee, K. W., Gil, Y. C., …Tansatit, T., Kim, H. J. (2021). Three-dimensional evaluation of the depressor anguli oris and depressor labii inferioris for botulinum toxin injections. Aesthetic Surgery Journal, 41(6), NP456–NP461. https://doi.org/10.1093/asj/sjaa083

Ultrasound evaluation of arterial anastomosis of the forehead (2018)
Title : Ultrasound evaluation of arterial anastomosis of the forehead
Researcher : Tansatit, T., Phumyoo, T., Jitaree, B., Sawatwong, W., Rungsawang, C., Sahraoui, Y.M.E.,… Lee, J.H.
Abstract : Background: Color Doppler ultrasound has a potential role as an imaging guide in aiding filler injections which are blinded procedures.
Objective: This study investigated the forehead arteries and provided insight into their anastomoses. This was performed by challenging their function to provide blood through these anastomoses when the main artery was temporary occluded by compression.
Methods: Three arteries were identified on each side of the forehead, the supratrochlear, the supraorbital and the superficial temporal arteries. Under ultrasound monitoring, each target artery and corresponding anastomosis was studied separately by compressions performed in a sequential and accumulative manner.
Results: Data from the current study imply that accidental cannulation of either the supratrochlear artery or the supraorbital artery can cause ophthalmic artery embolization in every case recorded. If the frontal branch of the superficial temporal artery is cannulated, the chance of blindness as a complication occurs in one fifth of volunteers. Anastomosis between both sides of the terminal branches of ophthalmic arteries creates the possibility of bilateral ocular complications when accidental cannulation occurs at one of these branches, especially the supratrochlear artery. Thus, injury to the supratrochlear artery carries a greater risk of complication than the supraorbital artery.
Conclusion: These findings emphasize that the chance of ocular complication is less when accidental cannulation occurs at the superficial temporal artery compared with injury to the supratrochlear or the supraorbital arteries as the terminal branches of the ophthalmic artery. Ultrasound can assist in the identification and evaluation of all the arteries at risk, thus avoiding the occurrence of vascular complications.
Link to Academic article: https://doi.org/10.1111/jocd.12755
Journal : Journal of Cosmetic Dermatology, 2018, 17(6).
Bibliography : Tansatit, T., Phumyoo, T., Jitaree, B., Sawatwong, W., Rungsawang, C., Jiirasutat, N.,…Lee, J. H. (2018). Ultrasound evaluation of arterial anastomosis of the forehead. Journal of Cosmetic Dermatology, 17(6), 1031–1036.